MAPS-MCRC Community Health Clinic
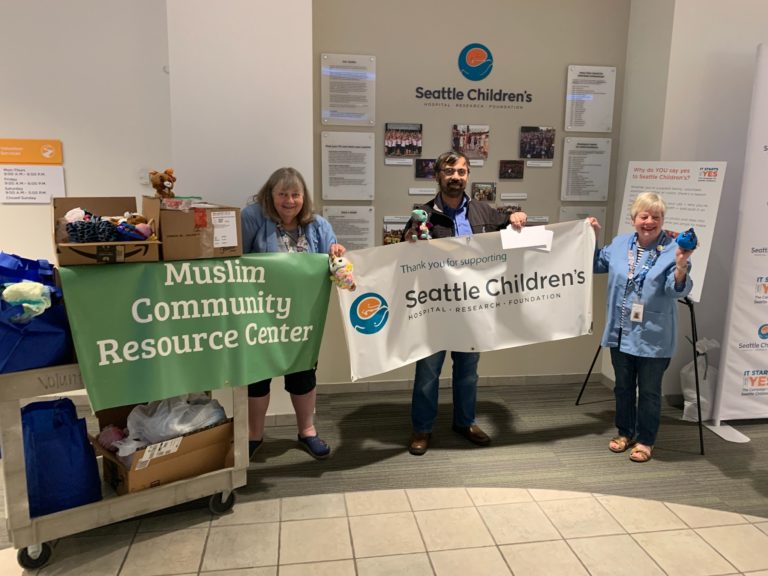
MAPS-MCRC Clinic is a fully volunteer run, mosque-based free clinic located in Redmond, WA to meet the healthcare needs of the community regardless of race, religion, and ability to pay. The clinic is part of a network of safety net clinics linked by the Washington Healthcare Access Alliance. Since its opening in 2016, the clinic has seen approximately 530 patients, both in-person and telehealth. Since April 2020, the clinic has been running virtually. Most patients are are recent immigrants, asylum seekers, uninsured, or are experiencing homelessness.
ESTABLISHING THE CLINIC
While Washington State has expanded Medicaid to cover many uninsured individuals, health care access still poses a challenge for those who are homeless, individuals who are undocumented, new immigrants, and/or travelers without insurance.
In 2016, Nehath Sheriff, MAPS-MCRC Community Clinic Director mobilized a monthly medical clinic Redmond, WA to meet an identified need for low-cost, quality care in the community. The clinic aims to leverage existing community resources to create a comprehensive care clinic, which provides healthcare services to individuals and families in need.
The clinic is operated at the Muslim Association of Puget Sound (MAPS) by the Muslim Community Resource Center (MCRC), which is the social and humanitarian program of MAPS.





ESTABLISHED
VOLUNTEER PHYSICIANS
COMMUNITY VOLUNTEERS
PATIENTS
2016
18
30+
530+







MODEL OF CARE
- Wellness Exams and Screenings
- Education and Prevention
- Continuity of Care
- Referrals to SDOH Resources
- At least one primary care physician at every clinic
- On-site lab: Blood pressure, HbA1c, lipid panels, etc.
- Physical examinations
- Specialty care (cardiology, neurology, endocrinology)
- Behavioral health services
- Flu shots/immunizations
- Culturally competent healthcare delivery (e.g., diverse providers, language resources, etc.)
- Health insurance enrollment
- On-site social services (e.g., financial aid, medication management, etc.)
- Follow-up: patients deemed high-risk are contacted weekly until they have established continuity of care or can be seen at the clinic again.
The clinic’s goal is to establish continuity of care while connecting patients to local resources that can improve care. This can include:
- Having volunteer physicians see patients in their own clinics
- Connecting patients to hospitals that provide charity care
- Referring patients to community clinics that operate daily
Before patients leave the clinic, they are given referrals to known community resources based on identified social determinants of health. Examples of referrals include:
- Food pantries that meet dietary needs
- Connections to local shelters or housing agencies
- Transportation to and from the clinic
STAFFING STRUCTURE
Pre-COVID, the clinic operated monthly and was fully staffed through a rotating team of volunteers. All volunteers are required to undergo mandatory HIPAA training.
The Washington Healthcare Access Alliance’s (WHAA) Volunteer and Retired Provider (VRP) program covers every provider with $1 million in malpractice insurance. The VRP program ensures that all providers are licensed by WA, have completed the necessary training (e.g., residency) and are qualified to be treating patients at the clinic. Being part of the WHAA guarantees that patients (and providers) who rely on referrals to safety net clinics have an expansive network.
-
Physician (MD/DO/ND)
Must be licensed in Washington State (i.e., completion of medical residency) and fully insured under the WHAA.
-
Nurse (RN, LNP)
Licensed professional in WA State and fully insured under the WHAA.
-
Clinic Director
Directs clinic logistics, communicates with both providers and patients, primary point of contact for all clinic needs and handles patient follow-up and pharmacy calls.
-
Clinic Manager
Manages day-to-day operations and volunteers and is responsible for on-site lab and related deliveries.
-
Runner
Facilitate communications between clinic staff and patients.
-
Hygienist
Maintain a clean and safe environment for patient care.
-
Scribe
Input patient data and support MAs and/or physicians with patient information.
-
Patient Navigator
Registration, first and last point of contact for patients, help facilitate development of health records and provide patients with community resources as needed.
-
Data Analytics
Ongoing data evaluation, analysis and compiling patient data to improve care.
COMMUNITY CARE DURING COVID-19
- Services reconfigured to safely reach the vulnerable populations by offering free weekly telehealth services
- Provided free COVID-19 Testing at the height of the COVID-19 pandemic in Washington
- Distributed PPE to First Responders and vulnerable groups when there was a shortage of masks and PPE
- Collaborated with Albertson’s Group of Pharmacies to provide COVID-19 vaccine for individuals in phase 1A & 1B of the Washington State vaccine rollout.
- Making MAPS facility available as mass vaccination site
MENTAL HEALTH SERVICES
- Weekly “Mindful Tuesday” webinars with a licensed clinical social worker that covers pertinent issues for the community. Examples include anxiety, depression, setting healthy boundaries, building healthy relationships, etc.
- Virtual Emotional Wellness Consultations with Yassir Fazaga, a licensed clinical social worker and Muslim scholar, aims to directly address the mental health needs of the community
- Partnership with NAMI (National Alliance on Mental Illness) Eastside to create (virtual) group mental health sessions
PAYER MIX
During the pilot phase (year 1) it was proposed that the clinic provide services on a sliding scale. During subsequent years, the financial model has shifted due to the unique payer mix. Over 90% of utilizers of MAPS-MCRC Clinic do not have insurance (e.g., commercial, Medicaid, Medicare, or traveler’s). Today, patients are treated at no-cost but are asked to donate any desired amount. Money accrued from all billable insurance is used only for clinic operations.
MONITORING AND EVALUATION
Clinic’s evolution is data-driven through ongoing monitoring and evaluation. A data team monitors patient intake forms and surveys both physicians and patients to understand needs. Some of the ways in which the clinic’s operations have adapted based on results are:
- Incorporating in-house behavioral health (BH) services.
- Developing a provider volunteer team that covers the needs identified by high-utilizers of our clinic.
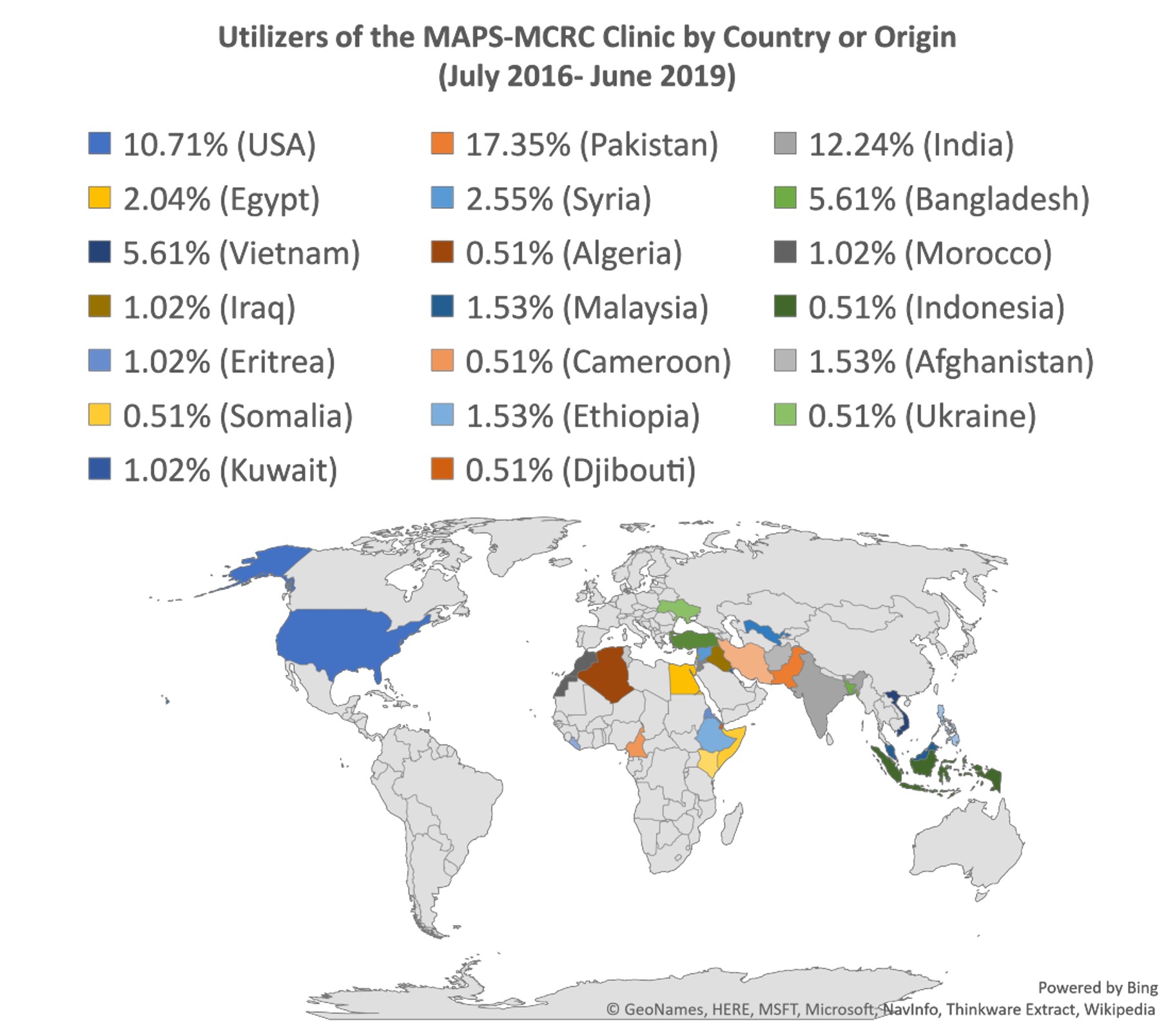
- Enhancing culturally-relevant approaches to care. This is especially important given the diversity of the clinic’s patient population. As shown in the figure, the vast majority of the utilizers were born outside of the United States.*
*24.5% of patients chose not to respond to the survey question regarding country of origin.
DEMOGRAPHIC DATA
Our data has shown:
- Gender identity: 68%/70.4% female and 28%/29.6% male
- 71% of our patients are not U.S. citizens (we do not ask for immigration status)
- Our patients speak over 15 different languages
- Language: 57.3% of patients speak a language other than English; 30.3% speak English fluently; and 12.4% chose not to answer.
- Patients originate from over 35 different countries
- Race: 49% are Asian; 9% African American; 24% Caucasian; 3% African; 15% declined to answer.
- Citizenship: 34.8% are U.S. citizens
- Average age: 51.7/51.5 years old
- The average education level is a 4-year university
- Religion: 53% of our patients are Muslim
- Upon registration, all patients are asked to fill out an optional questionnaire. Many choose not to answer, either due to comfort, time limits, or language barriers.
- Many patients prefer to see a provider who shares their gender identity. In recruiting volunteer healthcare providers, the clinic strives to accommodate this preference.
- Currently, the majority of the volunteer physicians are female.
- The race/ethnicity distribution of the clinic’s physician team is also well-matched with the patient mix. Out of 18 rotating physicians, 15 physicians speak a language other than English.
(Note: the clinic is open to everyone, regardless of religion, race, insurance status, etc.)
NEXT STEPS
As the needs of the community grow, the clinic faces increased demand. From inception in July 2016 and mid-2019, MAPS-MCRC Community Health Clinic has cumulatively served over 300 unique patients, and the number grows with each monthly session.
The clinic is seeking to expand to full-time operation, but faces barriers such as:
- Physician availability
- Financial burden of scaling up and paying for a full-time clinician
Despite barriers, there are strong grounds for optimism regarding the scale-up:
- Availability of a full-time space in the current operating location
- Received a $75,000 grant supporting build-out of the clinic
- Community members willing to further invest in the infrastructure
- In conversation with regulators regarding becoming a Federally Qualified Health Center (FQHC) or FQHC look-alike
- Retired healthcare providers willing to work full-time at the clinic